(USMLE topics) ACS: Symptoms, risk factors, causes, pathophysiology, diagnosis (ECG and cardiac markers), treatments. This video is available for instant download licensing here: https://www.alilamedicalmedia.com/-/galleries/narrated-videos-by-topics/cardiac-pathology/-/medias/30984947-aca5-453d-b1ae-f3a9e1f6a07d-acute-coronary-syndrome-acs-unstable-angina-nstemi-and-stem Voice by: Marty Henne ©Alila Medical Media. All rights reserved. Support us on Patreon and get early access to videos and free image downloads: patreon.com/AlilaMedicalMedia All images/videos by Alila Medical Media are for information purposes ONLY and are NOT intended to replace professional medical advice, diagnosis or treatment. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition. Acute coronary syndrome, ACS, is a group of conditions that occur when blood supply to an area of the heart muscle, the myocardium, is suddenly reduced or blocked. Reduced blood supply is termed ischemia. A prolonged ischemia can lead to death of the heart tissue, known as heart attack or myocardial infarction. A typical symptom of ACS is central chest pain or discomfort that may spread to the back, jaw, left shoulder or arm. The pain may also be felt in the abdomen and can be mistaken for indigestion. Other symptoms include shortness of breath, heavy sweating, nausea, palpitations, and fainting. Women and older people often have atypical symptoms. Chest pain is not reported in about 30% of cases. About 20% of patients have mild or no symptoms. Risk factors include: aging, family history of heart diseases, smoking, diabetes, hypertension, high cholesterol, obesity, sedentary lifestyle, unhealthy diets, and psychosocial stress. The most common cause of ACS is the formation of a blood clot in an artery already narrowed by an atherosclerotic plaque. Plaques are deposits of lipids, fibrous tissue and calcium, that accumulate slowly overtime. A plaque may become inflamed and rupture, exposing substances that promote coagulation, producing a blood clot on top of the plaque. Less common causes include coronary artery embolism, coronary spasms, and coronary artery dissection. Depending on the location and the extent of obstruction, one of the following conditions may result: – Unstable angina, – Non-ST-segment elevation myocardial infarction, NSTEMI, – Or ST-segment elevation myocardial infarction, STEMI. These conditions are differentiated based on ECG findings and cardiac marker levels. Markers are substances released into the bloodstream upon death of cardiac myocytes. Cardiac troponins are the markers of choice as they become elevated early in the disease process. The amount of troponin released is proportional to the infarct size. Most patients with infarction show elevated troponin levels within 6 hours. Troponin assay is usually done on presentation and then repeated a few hours later. Unstable angina is basically ischemia without infraction. It impairs cardiac function but has not caused cell death. ECG changes are absent or transient. Cardiac troponin levels remain normal, or only slightly elevated. It should be noted, however, that this condition is clinically unstable and often precedes a myocardial infarction. NSTEMI is infraction that is limited to the inner layer of the ventricular wall. Cardiac marker levels are elevated as a result of myocardial cell death. ECG changes may include ST-segment depression, or T-wave inversion, but not ST-segment elevation. STEMI is infarction that extends the entire thickness of the myocardium. STEMI results from a complete and persistent occlusion of blood flow. ECG findings show a characteristic ST-segment elevation. There is usually a reciprocal ST depression in the electrically opposite leads. The location of infarction can be identified based on the leads with ST elevation. Cardiac markers are elevated. All patients with suspected ACS are treated promptly with antiplatelets (usually aspirin), angina medications (usually nitroglycerin) and supplemental oxygen if required. Once diagnosis is confirmed, anticoagulants, beta-blockers, ACE inhibitors, and statin are usually initiated within 24 hours unless otherwise contraindicated. For STEMI patients, emergency percutaneous coronary intervention, PCI, is the preferred procedure to restore blood flow. If PCI is not available, a fibrinolytic therapy is usually initiated at the earliest possible time. For patients with unstable angina or NSTEMI, an angiography to identify sites of blockage may be done within 24 to 48 hours if the patient is clinically stable and the case is uncomplicated. For complicated cases, angiography must be done immediately. Fibrinolytic therapies are not indicated for NSTEMI patients.
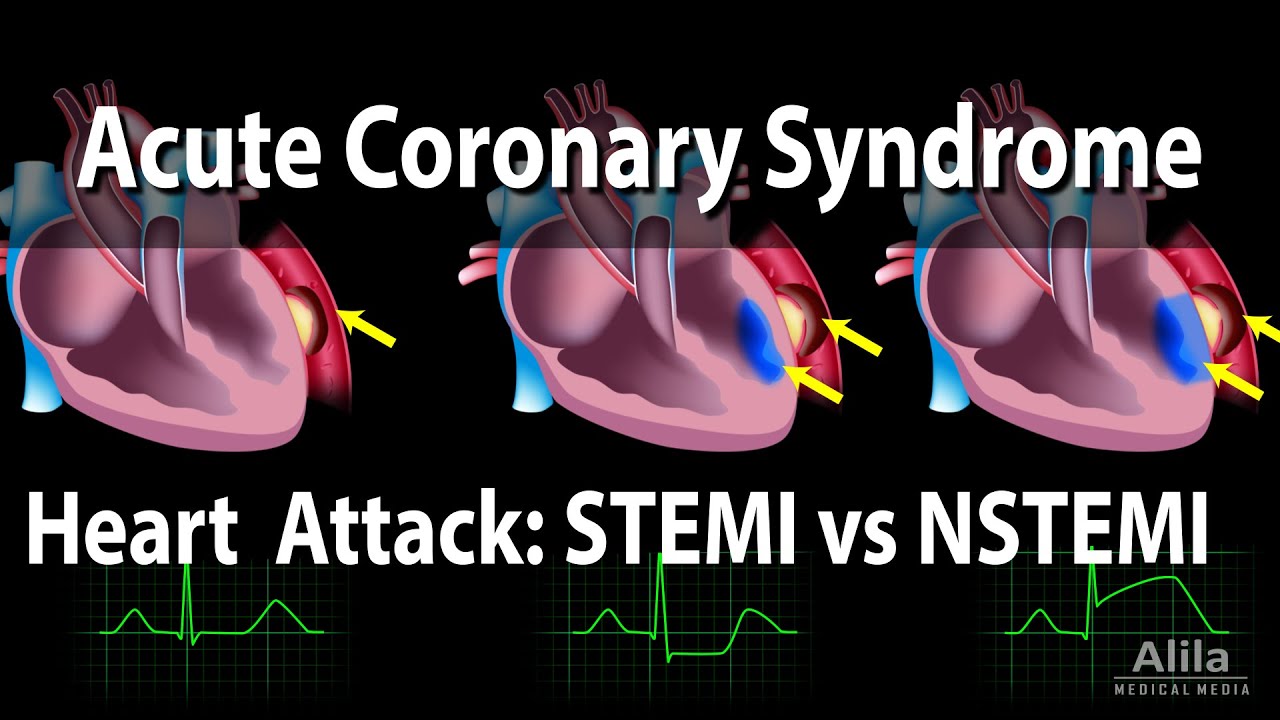
Acute Coronary Syndrome: Unstable Angina, NSTEMI and STEMI (Heart Attack), Animation
- Post author:admin
- Post published:October 7, 2021
- Post category:Uncategorized
- Post comments:0 Comments
You Might Also Like
When His Penis Won’t Stand Up: Causes of Erectile Dysfunction | Quint Fit

Testosterone & Androgenic Effects Video – 5

CREATINE ON CUTTING (क्रेटीने और कटिंग)- Does water retention |Causes bloating|

Best in class Multivitamin – Healthkart Multivit Gold, Clinically studied

Cardio Exercise Video – 1
Do You Know The Warning Signs of Heart Disease?
Yoga Counciling Video – 5

Sugar Free, Low Sugar Video – 1
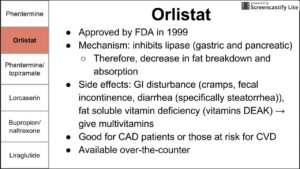
Anti-obesity medication

Human Body, Body Building Muscle Building Anatomy Physiology Video – 49

WiLD Soul Flow :: Primal Squat + Kneeling Arms & Low Lunge Sequence

Learning Disability Video – 2

DUMBBELL FLYES – HOW TO DO IT RIGHT

Functions Of Fat – How The Body Uses Fats – Importance Of Fats In The Body Explained

Running Muscle Groups used
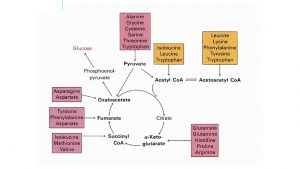
Bridge between Anabolic and Catabolic Pathways
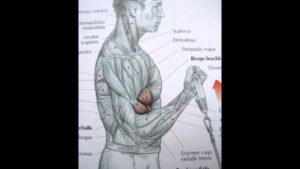
Bodybuilding: Biceps exercise and anatomy
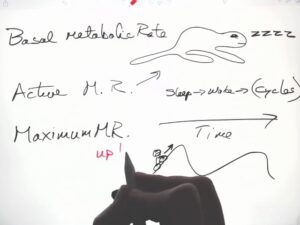
Energy Metabolism PART 2 BMR

Do Supplemental Vitamins Actually Work?

Nephrology Video – 4

Marathon Video – 4
BODYBUILDING MOTIVATION ~ This will Destroy you
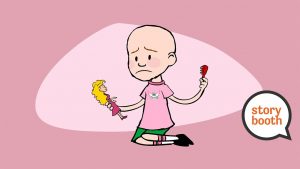
I Lost My Hair

Nutrition Plan and Supplementation Guide | Clutch Life: Ashley Conrad’s 24/7 Fitness Trainer
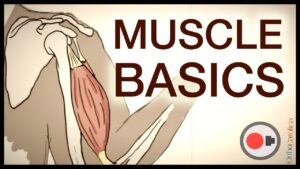
Human Body, Body Building Muscle Building Anatomy Physiology Video – 6

Glycine The Best Amino Acid✔️
Developmental Psychology Video – 2

The Onset X3-C from Fujifilm

Definition of repetition
JM PRESS: Skullcrusher + Close Grip Bench Hybrid- Effective and Safe Tricep Exercise

Sports Physiotherapy Video – 9
Nutrition
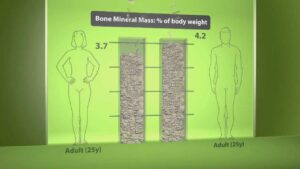
Human body composition

Long bone formation

Intermittent Fasting & Fasting Video – 3

BICEP EXERCISES FOR STRENGTH & DEFINITION

What Happens When You Take Steroids? | Earth Lab

Honey Nutrition Video – 2
Dumbbell Chest Workout (INCOMPLETE WITHOUT THIS!)

“Dumbbell Row” Exercise for Back Muscles

Why You Got Fat