medskl.com is a global, free open access medical education (FOAMEd) project covering the fundamentals of clinical medicine with animations, lectures and concise summaries. medskl.com is working with over 170 award-winning medical school professors to provide content in 200+ clinical presentations for use in the classroom and for physician CME. Psychiatry – Addiction/Substance Abuse: What You Cannot Afford to Miss Whiteboard Animation Transcript with Margaret S. Chisolm, MD https://medskl.com/Module/Index/addiction-substance-abuse When evaluating any patient, you cannot afford to miss substance abuse. Although not all patients will require specialty treatment, they can still benefit from your intervention. With every patient, here are some important steps to take: • Raise the subject: “Can we take a minute to discuss alcohol?” • Ask about use: “Do you sometimes drink beer, wine, or liquor?” • If the response is “No,” ask: “Why not?” • If “Yes,” ask: “How many times in the past 12 months have you had X or more drinks in one day? For men, X = 5; for women and anyone over age 65, X=4. • If the answer is anything other than “zero,” this is a sign of risky drinking and a brief intervention is indicated, as follows. BRIEF INTERVENTION Provide feedback. • Share that level of use exceeds lower risk limits established for healthy men and women. • Let your patient know that drinking at this level can be unhealthy. • If possible, connect risk to reason for the visit: “I think your insomnia may be related to drinking.” Enhance motivation. • Ask questions that elicit change talk: “Have you ever considered cutting down or quitting?” • If so, “Why?” • If not, ““What would have to happen for you to consider it?” • Ask the patient to rate the importance of change, using a visual “readiness ruler” if possible: • “On a scale of 1-10, how important is it that you cut down or quit?” • Then ask: “Why [that number] and not a lower one?” Negotiate a plan. • Next steps should be developed collaboratively. • Follow the patient’s lead: “If you were to make a change, what would be the first step?” • Offer a menu of options for more help such as medication, brief counselling, support groups, and/or formal treatment programs. Close on good terms. • Ask permission to meet again to discuss progress.

Addiction Psychiatry Video – 1
- Post author:admin
- Post published:May 18, 2021
- Post category:Uncategorized
- Post comments:0 Comments
You Might Also Like
thyroid gland and hormone synthesis
What is Adenomyosis? (Enlarged Uterus)
Preparation for a BodyBuilding Competition – 20 WEEKS OUT! World Champion Explains

How To: Close-Grip Barbell Bench Press

Barbell Bench Press – HASfit Chest Exercise Demonstration – Flat Bench Presses Form – Pectoral

Hair Loss Treatment for Men / Male Pattern Baldness Treatment – FUE Hair Transplant Result

What does Telmisartan do?
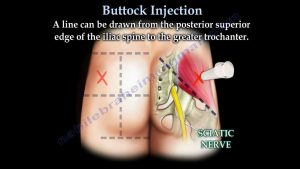
Buttock Injection – Everything You Need To Know – Dr. Nabil Ebraheim

Is BCCA Good For Your Body? | BeerBiceps BCAA 101

Thyroid Hormone Resistance Workshop
What causes diabetes, high blood sugar and type 2 diabetes
![Read more about the article WHICH IS THE BEST INDIAN SUPPLEMENT BRAND FOR RESULTS [CLOSED]](https://videos.drmaheshkumar.com/wp-content/uploads/2021/05/WHICH-IS-THE-BEST-INDIAN-SUPPLEMENT-BRAND-FOR-RESULTS-CLOSED-1-300x169.jpg)
WHICH IS THE BEST INDIAN SUPPLEMENT BRAND FOR RESULTS [CLOSED]
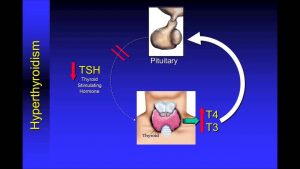
Understanding Thyroid Function Tests
Difference Between Adverse Effect and Side Effect
Isis Module 1 Animation How Antisense Drugs Work

Personal Trainer/ Gym Instructor Video – 5
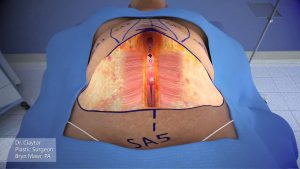
Dr Claytor demonstrates tummy tuck with liposuction 3 D animation: No Drains
What are metabolic processes
Dr. Drew talks finasteride warnings

Popping Sound during Joint Adjustment | Chiropractic Care
Jogging

Things you must know before taking Glutamine Supplements | HINDI
What is Heart Attack explained in Hindi by Dr. Vinod Sharma.

How To Cool Down After Exercise

Bone Cancer – 7 Warning Signs
Making A Yoga Routine Video – 2
Protein Requirement According To Workout

Lose Thigh Fat in 2 weeks – Easy thigh exercise & workout to get slim legs
“Nutrition 101” with Dr. Charles Mok

Latissimus Dorsi Bent Over Row-11

Back Extension…You’re Doing It WRONG
Protective Medicines

The Best Pre-Workout Meal for Muscle Gain
Normal Sinus Rhythm ECG – EMTprep.com

Erin Stern Shoulder Workout for Rear Delts

What is renal hypertension? – Ask ADC video
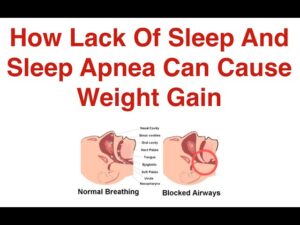
How Lack Of Sleep And Sleep Apnea Can Cause Weight Gain
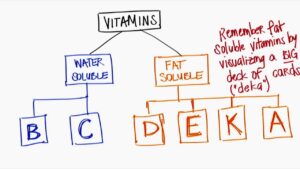
Fat & Water Soluble Vitamins!

Killer Leg Toning Workouts You Can Do At Home – Short home workout routine

Badminton Video – 1
Sugar Free, Low Sugar Video – 26