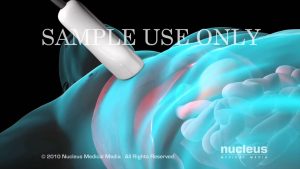
Intracytoplasmic sperm injection, or ICSI, is a form of in vitro fertilization in which fertilization occurs outside of the body. First, egg cells are harvested and transferred to a special media in a laboratory dish. Within a few hours, a single sperm is injected through a fine needle into the center of an egg cell to aid in the process of fertilization. If successful, the cell will divide and form the beginning stages of an embryo. If necessary, the DNA of a single cell from an embryo may be checked to ensure that various genetic disorders are not present. Typically, several egg cells are harvested and fertilized at the same time then inserted back into the uterus to increase the chances that one will implant and develop into a successful pregnancy. Intracytoplasmic sperm injection (ICSI) is an in vitro fertilization procedure in which a single sperm is injected directly into an egg. Indications Schematic image of intracytoplasmic sperm injection in the context of IVF. This procedure is most commonly used to overcome male infertility problems, although it may also be used where eggs cannot easily be penetrated by sperm, and occasionally in addition to sperm donation. It can be used in teratozoospermia, because once the egg is fertilized, abnormal sperm morphology does not appear to influence blastocyst development or blastocyst morphology.[2] Even with severe teratozoospermia, microscopy can still detect the few sperm cells that have a “normal” morphology, allowing for optimal success rate. History The first gamete micromanipulation techniques date back to the late 50’s. In Rome in 1990 there was the first birth by injection of the sperm into the perivitelline space (SUZI) obtained by the team Simon Fishel, Severino Antinori and Franco Lisi. The technique was developed by Gianpiero Palermo in 1991 at the Vrije Universiteit Brussel, in the Center for Reproductive Medicine headed by Paul Devroey and Andre Van Steirteghem.[3] The first American baby was conceived with the technique At Reproductive Biology Associates (RBA) in Atlanta, Georgia in 1992 under the direction of Michael Tucker, PhD and Joe Massey, MD. ( ref. Case report, American Society for Reproductive Medicine, Abstract report at ASRM meeting, Montreal, Canada, 1993.) The first large experience with the technique in the United States was published by Joseph D. Schulman and colleagues at Genetics and IVF Institute in 1995. Procedure ICSI is generally performed following an in vitro fertilization procedure to extract one to several oocytes from a woman. The procedure is done under a microscope using multiple micromanipulation devices (micromanipulator, microinjectors and micropipettes). A holding pipette stabilizes the mature oocyte with gentle suction applied by a microinjector. From the opposite side a thin, hollow glass micropipette is used to collect a single sperm, having immobilised it by cutting its tail with the point of the micropipette. The oocyte is pierced through the oolemma and directed to the inner part of the oocyte (cytoplasm). The sperm is then released into the oocyte. The pictured oocyte has an extruded polar body at about 12 o’clock indicating its maturity. The polar body is positioned at the 12 or 6 o’clock position, to ensure that the inserted micropipette does not disrupt the spindle inside the egg. After the procedure, the oocyte will be placed into cell culture and checked on the following day for signs of fertilization. In contrast, in natural fertilization sperm compete and when the first sperm penetrates the oolemma, the oolemma hardens to block the entry of any other sperm. Concern has been raised that in ICSI this sperm selection process is bypassed and the sperm is selected by the embryologist without any specific testing. However, in mid-2006 the FDA cleared a device that allows embryologists to select mature sperm for ICSI based on sperm binding to hyaluronan, the main constituent of the gel layer (cumulus oophorus) surrounding the oocyte. The device provides microscopic droplets of hyaluronan hydrogel attached to the culture dish. The embryologist places the prepared sperm on the microdot, selects and captures sperm that bind to the dot. Basic research on the maturation of sperm shows that hyaluronan-binding sperm are more mature and show fewer DNA strand breaks and significantly lower levels of aneuploidy than the sperm population from which they were selected. A brand name for one such sperm selection device is PICSI.[5] A recent clinical trial showed a sharp reduction in miscarriage with embryos derived from PICSI sperm selection.
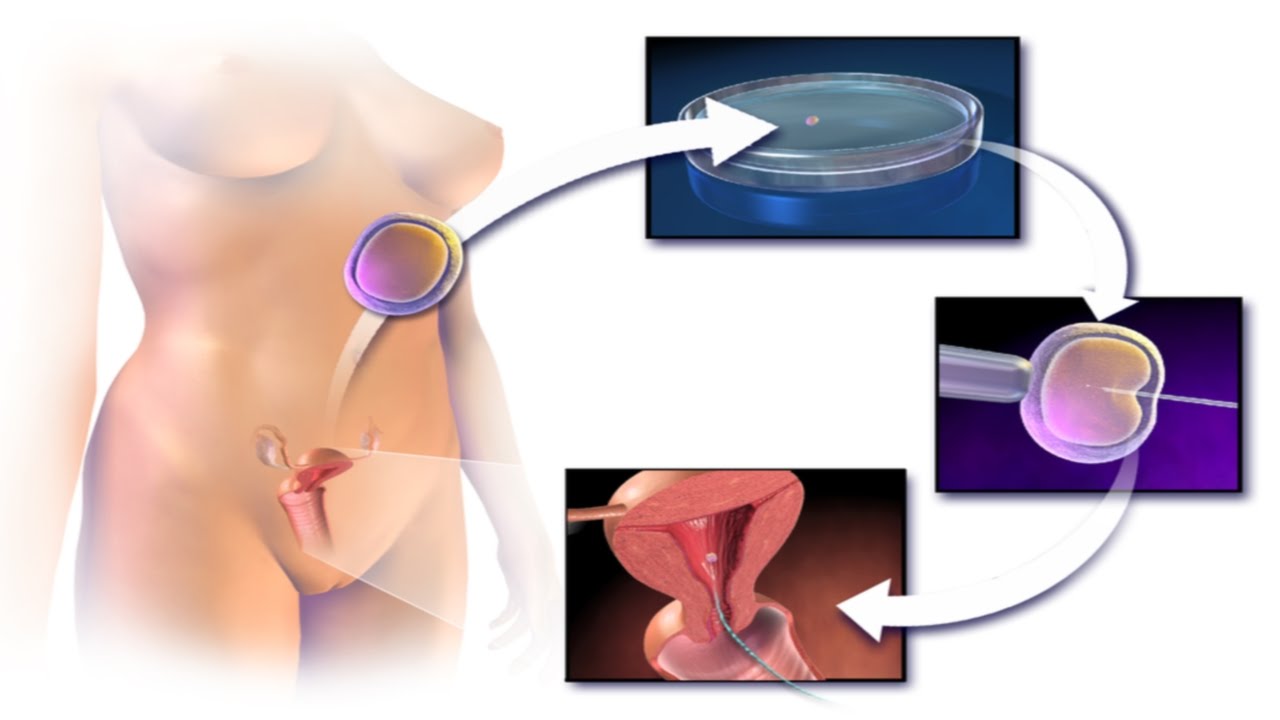
How to Get Pregnant with ICSI? Intracytoplasmic Sperm Injection Procedure Step by Step Video IVF
- Post author:
- Post published:May 25, 2021
- Post category:Uncategorized
- Post comments:0 Comments
You Might Also Like

Erector Spinae Back Extension-22

Sport Meaning

Micronutrition Pt 2 – Antioxidants and Phytochemicals

All about Creatine, Creatine side effects | hindi india | Bodybuilding lean muscular body

Basic Renal Function: Clearance and GFR

internal organs crunched

Bodybuilding Video – 1

Is the Traditional BMI Chart Accurate?
How to do Cable Bent Over Triceps Extensions? #91
7 Most Useful Antioxidants for Skin
Otorhinolaryngology Video – 3
Pregnancy

Body Mass Index, Health Eating and Weight Loss – Telugu

How to Deal With Morning Sickness During Pregnancy? | Dr. Jyoti Kala
Types of Jaundice in Newborn

Skeletal System And Asanas Video – 4
Love Psychology Video – 2

Cardio-Thoracic Physiotherapy Video – 13

The Scariest Side Effect of Pregnancy!

Can you get pregnant after an ectopic pregnancy | Quick Question
Liver Biopsy

Keto Diet, Keto Foods, Keto Recipes Video – 3

How to Make Minoxidil (Rogaine) More Effective

Standing Back Extension for Low Back Pain Relief

Trampoline Video – 2
![Read more about the article [Human Body 8] Make sure you know about FEVER](https://videos.drmaheshkumar.com/wp-content/uploads/2021/05/Human-Body-8-Make-sure-you-know-about-FEVER-300x169.jpg)
[Human Body 8] Make sure you know about FEVER

Andrology Video – 3

Critical Care Medicine Video – 3

Hyperextension With Machine-5

Pregnant? Help Protect Your Baby from Whooping Cough

Erector Spinae Back Extension-5

Community Psychiatry Video – 1
Graveyard Shift – Blood pools

Plank with Donkey Kick
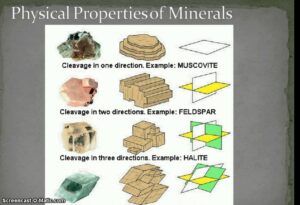
Mineral Cleavage
Asanas Meaning And More Asanas Video – 2

How to obtain: Apical 4 (Four) Chamber Ultrasound View- Training and Techniques – ICU
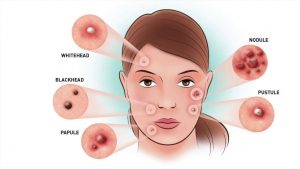
6 Different Types Of Pimples That You Should Know

Sports Physiotherapy Video – 13

Latissimus Dorsi Bent Over Row-5
Sleep & Insomnia Nutrition Video – 2