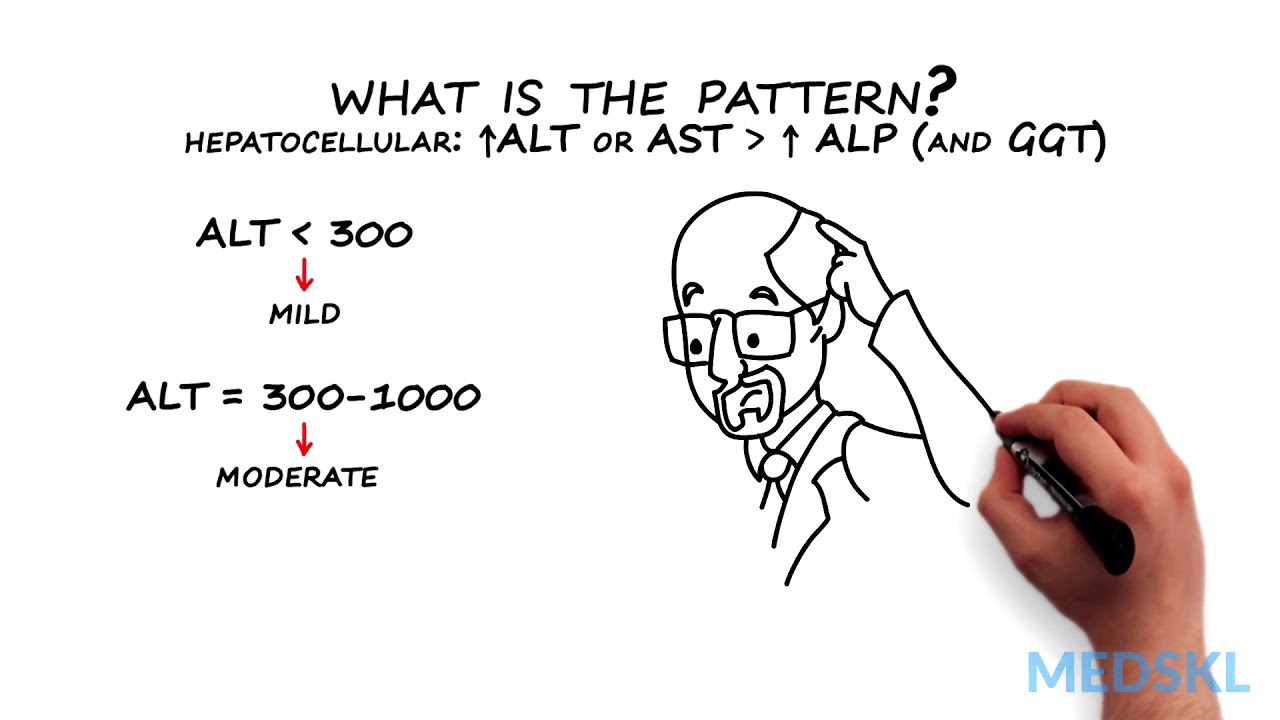
Abnormal liver tests occur frequently. Liver enzymes are frequently confused with liver function tests. This module will help distinguish the two. It is important to be able to assess the test results in light of the patient’s presenting complaint, risk factors and condition. This module will also cover an approach to patients with abnormal liver test results. medskl.com is a global, free open access medical education (FOAMEd) project covering the fundamentals of clinical medicine with animations, lectures and concise summaries. medskl.com is working with over 170 award-winning medical school professors to provide content in 200+ clinical presentations for use in the classroom and for physician CME. Gastroenterology – Abnormal Liver Tests Whiteboard Animation Transcript with Kelly Burak, MD https://medskl.com/module/index/abnormal-liver-tests INTRODUCTION Liver tests or liver enzymes, sometimes incorrectly call liver “function” tests, refer to AST, ALT, ALP, and may include GGT. Abnormal values are often found on routine blood tests and indicate liver injury. Bilirubin, albumin and prothrombin time (or INR) are better tests of the function of the liver and are the LFTs. How to Interpret Abnormal Liver Tests A patient with abnormal liver tests can present in a number of different ways or can be completely asymptomatic.1,2,3 While a clinical assessment focused on risk factors and stigmata of liver disease remains key, the pattern of liver enzyme elevation will guide the differential and workup. 1. Take a look at which enzymes are elevated. A rise in ALT and/or AST that is proportionally higher than ALP indicates a hepatocellular pattern of injury,1 while A rise in ALP, confirmed to be from liver by an abnormal GGT, indicates a cholestatic pattern.1 2. What is the pattern? If the pattern of injury is cholestatic – that is the ALP (and GGT) rise > ALT or AST – you will need to obtain a dedicated ultrasound of the liver and biliary tree to look at the bile ducts Dilated bile duct indicate extrahepatic cholestasis and an ERCP may be needed for diagnosis and therapy Normal bile ducts indicate intrahepatic cholestasis, and a liver biopsy may be required if the cause is not identified by history or other investigations, such as an anti-mitochondrial antibody or MRCP If the pattern of injury is hepatocellular – that is the ALT or AST rise is greater than ALP (and GGT) – determine severity using the ALT level An ALT of <300 is mild and 300-1000 correspond to moderate liver disease.1 These can be acute or chronic and unfortunately the differential diagnosis is broad Non Alcoholic Fatty Liver Disease (NAFLD) is the most common cause of mild elevation4,5 Alcoholic liver disease is associated with an AST that is often 2-3 times higher than the ALT, but alcohol or NAFLD rarely cause the ALT to be <3001,4,5 Further evaluation and testing will be guided by your history and clinical suspicion If ALT >1000 there is SEVERE liver injury which is always acute and symptomatic. These patients are at high risk of acute liver failure.1,3 If you see these values, think and test for the following: Drugs – especially acetaminophen overdose; Viruses – Hepatitis A through E, HSV, CMV, VZV; Ischemia from Budd-Chiari Syndrome or shock; Autoimmune Hepatitis; Wilson’s Disease; and if the patient is pregnant or recently postpartum, HELLP syndrome or acute fatty liver of pregnancy (AFLP)1,3 Quick recognition and diagnosis can guide appropriate management in these patients
Gastroenterology – Abnormal Liver Tests: By Kelly Burak M.D.
- Post author:
- Post published:June 6, 2021
- Post category:Uncategorized
- Post comments:0 Comments
You Might Also Like

How to get pregnant if male partner is having Erectile Dysfunction? – Dr. Basavaraj Devarashetty

2D echo: bubble study
Essential Fatty Acids – Efas Video – 2
HGH, Growth Hormones & Plant Hormones Video – 37

How to Do Lying Barbell Extensions

Close Grip Barbell Bench Press | Arm Workout

How to Get Rid of Varicose Veins Naturally – Varicose Veins Treatment

What is Kidney Disease?

Cricket Video – 4

One Arm Dumbbell Preacher Curls – Biceps Exercise – Bodybuilding.com
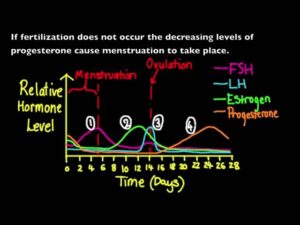
6.6.3 Annotate a graph showing hormone levels in the menstrual cycle
Why is water important for our bodies?

Aura Reading Video – 3

Barbell Shrug – upper back exercise correct form

Sports Nutrition Video – 1
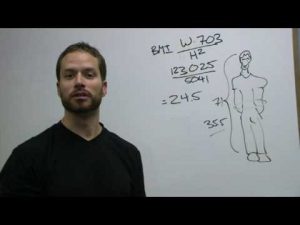
BMI – Calculating your BMI (Body Mass Index)

General Surgery Video – 1

What are your Strengths and Weaknesses? | interview questions & Answers

Spa Resort Video – 1
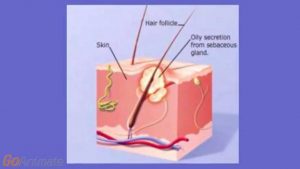
What is Acne and What is the Best Acne Treatment?

Close Grip Triceps Press

Organic Foods Video – 1

Antioxidant Content of 300 Foods

Joints: Crash Course A&P #20

Back Stability Ball Reverse Hyper Extension

Side Crunch With Weight-3

Anti-inflammatory antioxidants
What Is An Amino Acid? | Dr.Berg

Pec Fly Machine-1
The Human Body Video – 3

What Does Your Liver Do?

Love Psychology Video – 2

Anabolic Steroids – History, Definition, Use & Abuse Video – 22

Post ESWT Therapy on Frozen Shoulder
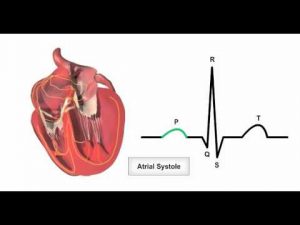
Anatomy & Physiology Online – Cardiac conduction system and its relationship with ECG

Detection of Urea in Urine – MeitY OLabs

L Glutamine Benefits and the Dangers!

The Ultimate Thyroid Home Test with Dr. Rob
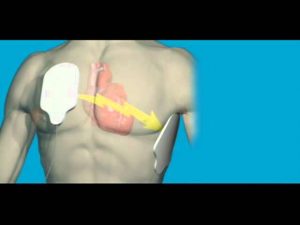
What is Cardiac Arrest

Deficiency & Malnutrition Video – 2

How to Do Back Extensions