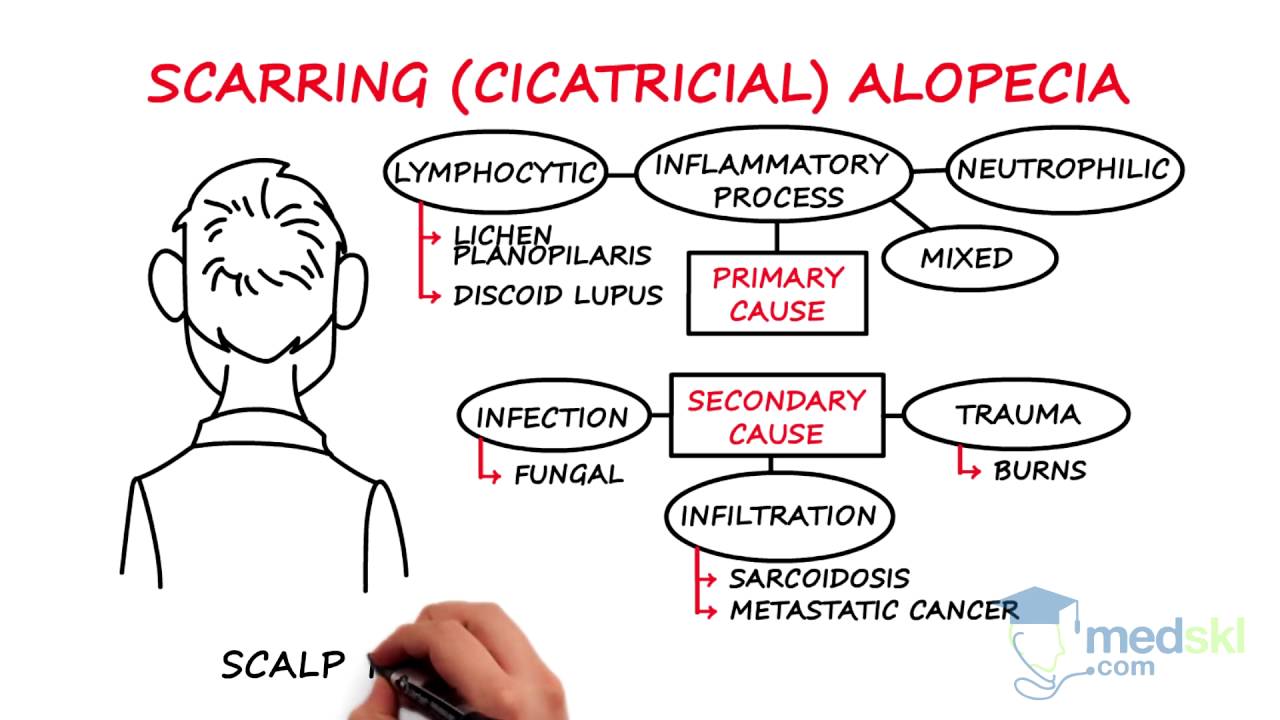
medskl.com is a free, global medical education site (FOAMEd) covering the fundamentals of clinical medicine with animations, lectures and concise summaries. medskl.com is working with over 170 award-winning medical school professors to provide content in 200+ clinical presentations. Dermatology – Alopecia: What You Need to Know Whiteboard Animation Transcript with Najwa Somani, MD https://medskl.com/Module/Index/alopecia Alopecia, or hair loss, can be broadly classified as scarring or non-scarring. In non-scarring alopecia, there is little to no inflammation or (as in alopecia areata) inflammation is directed at the non-permanent, cycling portion of the hair follicle (below the bulge – stem cell region). Scarring alopecia (aka cicatricial alopecia) is characterized by damage to the stem cell (bulge region) of the hair follicle resulting in fibrosis and permanent hair loss. Early dermatologic referral is imperative to prevent ongoing irreversible hair loss. Cicatricial alopecias are classified as primary or secondary. • In PRIMARY cicatricial alopecia, an inflammatory process specifically targets the hair follicle. These alopecias are classified according to the predominant inflammatory cell type and include entities such as lichen planopilaris and discoid lupus. • SECONDARY cicatricial alopecias involve infiltrative or inflammatory processes where the hair follicle is damaged secondarily. A scalp biopsy helps to guide optimal treatment. Depending on the subtype of cicatricial alopecia, clinically, one may see scar with loss of follicular ostia, tufting (where multiple hair fibers exit one ostia), erythema, scale, pustules, and sinus tracts. The main sub-types of non-scarring alopecias to be aware of are as follows: 1. Androgenetic alopecia is hormonally driven and presents with patterned hair loss. Topical minoxidil, antiandrogenic medications, and hair transplantation are typical treatments 2. Telogen effluvium is characterized by increased hair shedding and reduced hair density resulting from increased numbers of hairs shifting into a resting or telogen phase. Malnutrition, medications, endocrine abnormalities, and stress precipitate this shift. Management should address the underlying cause. 3. Alopecia areata is an autoimmune disorder presenting with smooth bald patches of hair loss on the scalp and sometimes on other body parts. Loss of all body hair is called alopecia universalis. It can be associated with other autoimmune disorders. Management includes topical and systemic immunomodulatory agents. Relapses are not infrequent. 4. Physical alopecias result from trauma to the hair follicle. This may be the consequence of traction from hairstyling practices, or due to an impulse-control disorder called trichotillomania, where individuals have a compulsion to pull out their hair. Patient education is key to management. Pharmacotherapy such as SSRIs may be required for trichotillomania.
Dermatology – Alopecia: By Najwa Somani M.D.
- Post author:
- Post published:May 23, 2021
- Post category:Uncategorized
- Post comments:0 Comments
You Might Also Like

Sciatic Pain | sciatica pain relief exercises | sciatic nerve

45 Hyper Extension Bench

Severe Liver Injury with Orlistat (Xenical, Alli)

How Much Fruit is Too Much Fruit?

Alternating hammer curls (standing with dumbbells)

Benefits of Omega 3 Fish Oil Supplements ft. Naturyz Triple Strength Omega 3 Fish Oil Supplement

What Does Your Liver Do?

Do You NEED Vitamin Supplements | Earth Lab

INTENSE Full Body Workout & Circuit Training – Get in Shape & Improve Overall Fitness
Andropause: Treating Male Hormone Imbalance Naturally (Male Menopause)

Shoulder Front Raise (w/ Band)
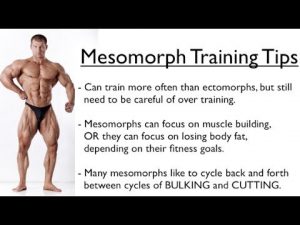
Ectomorph, Endomorph or Mesomorph – Training for YOUR Body Type
Isometric vs. Isotonic Contractions

Law 6: Optimize with a Pre-Workout | 10 Laws Of Muscle-Building

Dumbbell Row” Exercise for Back Muscles
The Skeletal System – Skeletal System Functions – Skeletal System Basics
GROWTH HORMONE INCREASE IN 3 SIMPLE WAYS |HGH vs INSULIN| (सीधी बात नो बक़वास) FULL EXPLANATION.

Hot Stone Therapy Video – 1
Elementary Physical Education – Fitness Components Stations
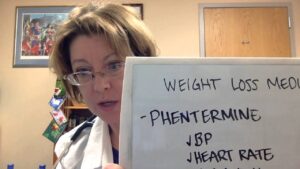
How To Lose Weight: Phentermine

MUSCULAR SYSTEM CONTRACTION AND RELAXATION CYCLE

Does Finasteride Only Work in the Crown?
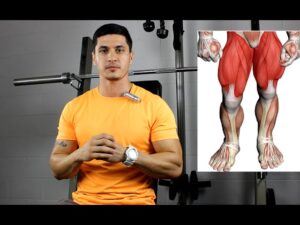
3 Quad Training Tips for Faster Leg Gains (Muscle-Group Series)

Angioplasty Procedure Animation Video.
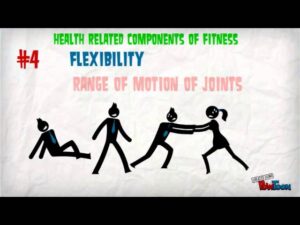
Health & Skill Components of Fitness
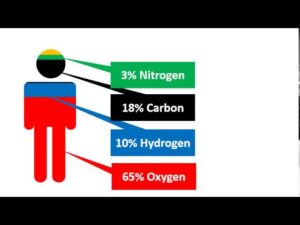
Elements of Life
What is Heart Attack explained in Hindi by Dr. Vinod Sharma.

Back extension / Hyperextension ( lower back exercises )

Overhead Press Dumbbells-4

What is the BEST WORKOUT FOR TEENS

Post-Workout Cooldown
Spiking insulin naturally to build muscle and lose fat

Pregnant Abdomen Examination (a.k.a. obstetric abdominal examination) – OSCE Guide

Medical Spa Club Video – 4

SIZE 8 – Post Workout Drink (NO Supplement) | Pure Vegetarian Muscle Building Program by Guru Mann

Clinical Psychology Video – 1

21 Inner thigh Exercises – Adductor Variations

Hormone Levels

TSA 9 Week Program Bench Progression
Echo Tech (Echocardiographic Technician) interview questions

Anabolic Steroids – History, Definition, Use & Abuse Video – 2