Hormonal treatments are used to help women ovulate or to help them “super-ovulate”, ovulate more than one egg. Women who do not ovulate spontaneously and have normal estradiol levels are traditionally prescribed Clomiphene Citrate, or Clomid. This medicine is a partial estrogen and partial anti-estrogen. Since 2003, stronger anti-estrogens, the aromatase inhibitors such as Letrozole, have become increasingly popular for ovulation induction. For women who don’t ovulate spontaneously, 80% will ovulate with clomiphene and 50% will conceive. Clomiphene Citrate is associated with multiple follicle growth, so twins and triplets may occur, 20% of pregnancies may be multiples. This medicine can have side effects such as hot flashes, sensitivity to light, headaches and mood swings. Also sometimes the cervical mucus is drier and thicker and sometimes the inside of the uterus doesn’t grow as thick as it should. Letrozole seems to have less side effects, is more likely to make more than one follicle, and the cervix and endometrium are less affected. In comparison studies, letrozole is as good as and maybe more effective than clomid for inducing ovulation. Letrozole has less birth defects compared with clomid in one comparison study. Both medicines are pills taken for 5 days after the start of a period. The pills are started between day 2 and 5. Dosage starts at one pill and can be increased in subsequent cycles to 2 pills or 3 pills as needed. Ovulation typically occurs one week after the last pill but may be later than that. For heavier women a higher dose or longer dose for up to 7 days may be the initial dose. For those with associated high testosterone levels, sometimes a low dose steroid, dexamethasone, can be added to the regimen to increase fertility. Insulin sensitizers such as metformin can also be added. When oral pills do not directly induce follicular growth, the next step has been ovulation induction with injectable pituitary hormones including FSH or a FSH/LH combination. The oral medications work by “tricking” the pituitary to produce more FSH to stimulate the ovary to make follicles. When this stimulus isn’t strong enough, the injectables provide the FSH directly to the ovary. These are usually successful but may produce multiple follicles. If there are too many follicles and the risk of multiple gestations is too high, then the cycle needs to be cancelled or converted into an IVF cycle where all the eggs can be removed and then we control how many embryos get transferred back in. Depending on the individual, doctors may use a combination of pills and shots that ultimately has a cost advantage and may work better than pills alone. Factors that may directly impact the success of these treatments are weight, diet and exercise. Weight is the biggest impediment to successful OI, especially with pills. A low calorie diet along with weight loss may help improve the odds of success. . A diet which included whole fat dairy is beneficial to fertility as is a plant based diet heavy in fruits and vegetables. Vigorous exercise may also improve a woman who was sedentary to ovulate. Of course some women don’t ovulate because they exercise too much. For some, weight loss is needed, however, for others weight gain, especially in body fat, is needed to ovulate. It is ultimately extremely important to discuss your individual situation with your doctor to create the best treatment option for you to produce your ideal results.

Infertility Hormonal Treatments • WCWRC
- Post author:
- Post published:May 30, 2021
- Post comments:0 Comments
You Might Also Like
Uterus and ovaries (preview) – Human Anatomy | Kenhub

Behavioral Psychology Video – 4
Side Effects of eating RAW EGGS | Info by Guru Mann

Spa Products Video – 3

Risk Associated With Iron Supplements

Target INNER Pecs – 3 Flat Dumbbell Chest Exercises

General Practice Video – 2

Full day Diet Plan to GAIN WEIGHT for Beginners! (Hindi / Punjabi)

TOP 5 Inner Thigh Exercises for Women (Strong Adductors!)

Stability-Ball Back Extension – Unleash Your Hottest Body
Kidney disease – Causes and treatment of kidney failure
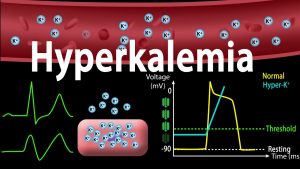
Hyperkalemia: Causes, Effects on the Heart, Pathophysiology, Treatment, Animation.

What are the side effects of fish oil for dogs?

Sugar Free, Low Sugar Video – 6
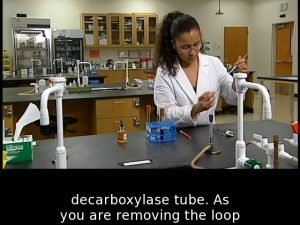
amino acid catabolism

BEST Workout & Diet ADVICE for SKINNY GUYS ft. Mike Matthews | How to Build & Gain Muscle FAST

Science Says Decline Dumbbell Bench Press Is BEST Chest Exercise

Cable V Bar Preacher Curls

5 Minute Butt and Thigh Workout for a Bigger Butt – Exercises to Lift and Tone Your Butt and Thighs

FAT Talk: Let’s talk about FAT and how to avoid too much of it!

Essential Oils Video – 4

Arthritis – Causes, Symptoms and Treatment Options
Fat Loss & Obesity
Anabolic Steroids – History, Definition, Use & Abuse
Cholesterol Lipid Panel Screening Procedure
How To Say Enalapril

Health Benefits of Fish Oil Omega-3 Fatty Acids | GuruMann

Reduce hips and thighs and tone up with this workout || Ashtrixx

Pec Fly Machine-2

Deltoid Front Raises-1

Testosterone & Androgenic Effects Video – 26

What is Fitness: Health & Skill Fitness Components PE

Skeletal System And Asanas Video – 2
![Read more about the article Pantoprazole; Errors, Side Effects, & What to Do [Doctor Interview]](https://videos.drmaheshkumar.com/wp-content/uploads/2021/05/Pantoprazole-Errors-Side-Effects-What-to-Do-Doctor-Interview-1-300x225.jpg)
Pantoprazole; Errors, Side Effects, & What to Do [Doctor Interview]

What To Eat Before And After Your Workout To Maximize Fat Loss – With Thomas DeLauer
This ONE Exercise Fat Burning Workout Burns 18.3 cal Per Minute – Body weight – HIIT Home Workout

hypotension Treatment by Dr K Sreedhar
Graveyard Shift – Blood pools

Close Grip Tricep Push Downs

One Hand Triceps Extension-1
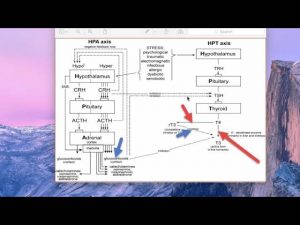
How your adrenal hormones affect thyroid and sex hormones