One unexpected and unwanted outcome from modernization of society is the increasing prevalence of diabetes mellitus due to changes in lifestyles. Diabetes is a lifelong disease which has no cure, causing terrible suffering among patients and tremendous strain on healthcare systems. Watch this episode of Medicurio to learn more about the cause, symptoms, and treatments available for diabetes. Rarer forms of Diabetes: Gestational Diabetes: Similar to Type 2 diabetes as some insulin resistance occurs, but only occurs during pregnancy. In most cases, gestational diabetes disappears once the baby is delivered, but some women progress into Type 2 diabetes even after birth. Likely due to various hormones released during pregnancy that interfere with the insulin signalling pathway, although the true cause is still being researched. Babies born to mothers with untreated gestational diabetes exhibit signs of Type 2 diabetes from birth. MODY (Maturity Onset Diabetes in Youth): Diabetes due to mutations in a MODY gene: a gene associated with either beta cell maturation, glucose storage and release, or insulin receptors. Specific symptoms and treatments vary based on the mutation, but all exhibit high blood glucose. There are currently 11 MODY genes known, but there are likely more that are undiscovered or too rare. Cool Links to check out: Diabetes Research Journals for up to date research on diabetes: http://diabetes.diabetesjournals.org/ http://www.canadianjournalofdiabetes.com/ Diabetes Canada: https://www.diabetes.ca/ Juvenile Diabetes Research Foundation (for Type 1 diabetes) http://www.jdrf.ca/ American Diabetes Association: http://www.diabetes.org/ Trivia: The first mention of diabetes occurred in Ancient Egypt over 3000 years ago, which described a sickness that caused excessive urination. This was likely Type 1 diabetes, as Type 2 diabetes only became more common when society and lifestyles became more modernized. One of the first ways to diagnose diabetes was to urinate on the ground and see if ants were attracted to the urine (which they would if it contained sugar). This was discovered in Ancient India. Insulin was discovered in Canada by Dr. Frederick Banting and his student Charles Best at the University of Toronto in 1920. They isolated the hormone from beagles and later injected diabetic beagles with their isolated substance, realizing that the hormone lowered blood glucose. This saved an innumerable amount of Type 1 diabetics’ lives, who rarely survived past childhood. Banting got the 1923 Nobel Prize in Medicine and Physiology that was shared with his supervisor, Dr. John Macleod. This decision infuriated Banting, who thought that Best should have shared the prize with him, and shared his cash award with Best. Initially, insulin was isolated from pig pancreas and then administered to patients. Over time, scientists managed to insert the gene for insulin into bacteria and yeast, which produced the hormone on a massive scale and allowed for more patients to be treated. Now, many different types of insulin are available. By slightly modifying the gene inserted into bacteria/yeast, and therefore modifying the insulin protein, scientists can control how fast insulin is broken down in the body. Fast-acting insulin can be administered right after a meal, while slow-acting insulin is administered before sleeping so that blood glucose levels can be maintained overnight.
Diabetes Mellitus and Insulin
- Post author:
- Post published:May 24, 2021
- Post category:Uncategorized
- Post comments:0 Comments
You Might Also Like

tablet capsule strip packing
Saturated Fat Explained (Made Easy to Understand)

Personal Trainer/ Gym Instructor Video – 5

CT Angiography with Dr. Arnder
Tadalafil (Cialis) for Erectile Dysfunction – 5mg, 10mg, 20mg – Uses, Dosage & Side Effects

Human Body, Body Building Muscle Building Anatomy Physiology Video – 37

Keto Diet, Keto Foods, Keto Recipes Video – 15
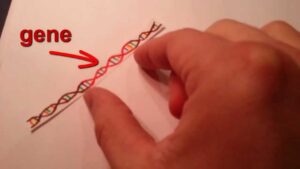
Gene Cloning in Plain English

Gastroenterology Video – 2
Sports

Leg Extension-2
Workout Stretching and Easy Warm Up Exercises – Static and Dynamic Stretching
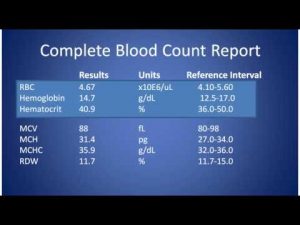
Complete Blood Count
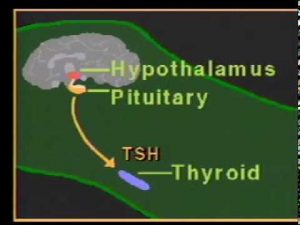
thyroid hormone physiology.mpg

One Arm Triceps Extension Bodybuilding Exercise

Crunches-5
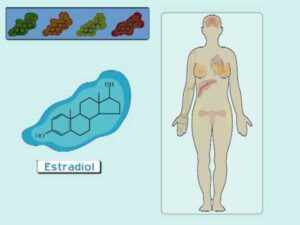
The Estrogen Receptor (I): Hormonal Mechanisms in the Body

Joe Rogan and Mark Sisson on Post Workout Shakes

Lower Back Exercise: Stability Ball Reverse Back Extension
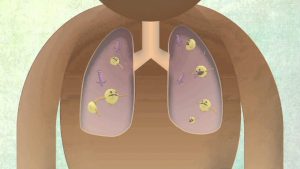
How The Body Reacts To Tuberculosis

Weight Loss Capsules in Pakistan 03244079761

Good Vitamin B Foods | Vitamins

Digestion in Human Beings 3D CBSE Class 7 Science (www.iDaaLearning.com)
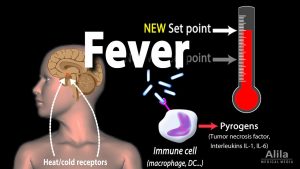
Induction of Fever, Control of Body Temperature, Hyperthermia, Animation.

Warning: Dangerous Fish Oil Omega 3 Side Effects

What Is Vitamin C? | Vitamins

Muscle Worship Growth

Pectoralis Pushups-7

01-Intro to A & P-definitions
Andropause: Treating Male Hormone Imbalance Naturally (Male Menopause)

Erector Spinae Back Extension-23
How The Body Uses Food – You Are What You Eat

Can testosterone supplements affect male fertility – Dr. Vasan S S

Pathology Video – 3

ENT Surgery Video – 2

Sugar Free, Low Sugar Video – 21

FULL FAT LOSS GROCERY HAUL (My Current Diet)

ARNOLD Training Back
ONDANSETRON
Erectile Dysfunction

Human Body, Body Building Muscle Building Anatomy Physiology Video – 46